In Vitro
What is an IVF procedure?The IVF procedure is individually prepared for every couple and depends on the medical history, laboratory test results and other factors. The physician recommends a treatment based on:
- hormonal tests results,
- ovarian reserve,
- woman’s age,
- obstetric and gynecological history,
- previous fertility treatments,
- US of ovaries.

Hormonal stimulation and monitoring
Ovarian stimulation during the IVF procedure aims to produce multiple eggs. Not every ovarian follicle growing during stimulation will contain a mature egg cell, and not every fertilized egg will be able to develop into an embryo. That is why mature eggs are required. As a result of stimulation, several eggs are collected.
Normally, hormonal stimulation takes 8 to 14 days. During ovarian stimulation, a woman takes medications to suppress her pituitary function, then gonadotropins to stimulate ovarian follicles growth. Monitoring with US and blood tests for hormone levels (estradiol, progesterone) is performed frequently.
The IVF cycle might be terminated before the retrieval, e.g. in situations when ovarian follicles no longer grow and develop. The older woman is, the more common such situation is. In such cases, the alternative strategy of medication is implemented.
Ovulation trigger on the last day of stimulation
Based on stimulation monitoring, the physician decides when ovarian follicles are mature (diameter 17-20 mm). On that day, the patient is given hCG injection, which induces ovulation. 36h after the injection, oocyte retrieval is performed.
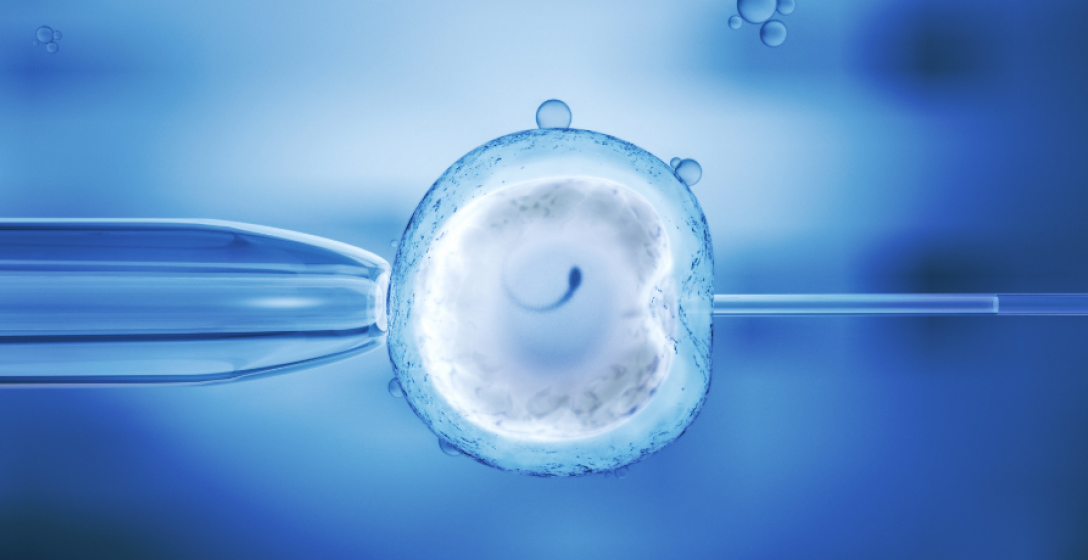
Oocyte retrieval – puncture
The procedure of mature eggs retrieval from ovaries is called ovarian puncture. The oocytes are retrieved by a needle through the vagina, under the control of US. The procedure does not require any other intervention in tissue other than a needle stick. The procedure is performed ~36h after hCG injection to induce ovulation.
The procedure lasts 10-20 min. and is usually performed under sedation, in the presence of a gynecologist and anesthetist. After the procedure, the collected follicular fluid containing oocytes is transported to the laboratory, and a patient is woken up. She spends ~1h in the recovery room.
On the day of puncture, some women feel cramps in the ovarian area. They disappear the day after. The pressure in the lower abdomen and pelvis may last for a couple of days because ovaries are still enlarged.
Fertilization and 5 days of embryo growth
After the eggs are retrieved from the fluid in the lab, their maturity and quality are evaluated. Fully mature cells are put in the special media and incubator, awaiting fertilization with the sperm.
Meanwhile, the sperm are isolated from the semen provided by the woman’s partner or anonymous donor (sperm bank).
Depending on recommendations, fertilization may be performed by:
- In Vitro Fertilization (IVF) – after the retrieval, eggs, and sperm are mixed and left in special conditions for the incubation process.
- Intracytoplasmic Sperm Injection (ICSI) – cumulus cells are removed, and single sperm is injected into each oocyte (microinjection).
- IMSI is an upgraded microinjection method – specially selected sperm of the quality and chances for conception is injected into each egg.
Fertilized oocytes are placed in an incubator at 37°C, high level of CO2 and a low level of O2.
In rare cases, fertilization may not be possible at all.
Embryo culture
~18 hours after the fertilization, the process is evaluated to check for any abnormalities. ICSI/IMSI increases the effectiveness up to 70-80%. The embryology team checks the embryos for the next couple of days. In each embryo, the number of cells and morphology are controlled.
Two days after the fertilization, the embryo normally has 2-4 cells; on the third day 6-10 cells.
On the fifth day, a cavity filled with fluid inside the embryo forms. Also, placenta and fetal cells start to form. From this point, the embryo is called a blastocyst.
Embryo transfer
After 3 to 5 days of embryo culture, 1 or 2 embryos are transferred to the woman’s uterus using a tiny catheter. The embryo transfer procedure is painless and is performed under ultrasound guidance. A full bladder is required. After the transfer, the patient lies flat for ~20 minutes.
If there are more embryos, it is suggested to transfer an embryo on the 5th day, when the embryo is in the mature stage of the blastocyst.
If the embryo develops correctly, it hatches out of the zona pellucida and implants in the endometrium. The implantation process ends between the 6th and 10th day after the retrieval.
ADDITIONAL EMBRYO TRANSFER OPTIONS:
- AH (assisted hatching) – zona pellucida is cut just before the transfer of the embryo. It aims to ease implantation in the endometrium.
- EMBRYO GLUE – a special substance supposed to improve the effectiveness of embryo implantation.
Embryo cryopreservation
All matured but not transferred embryos are cryopreserved. It is important to remember that not every embryo develops to the blastocyst stage. Not every blastocyst implants in the uterus and develops properly.
Correct embryos are preserved using the most effective method – vitrification – embryos are quickly brought to the temperature of liquid nitrogen (-196°C). Vitrification does not affect embryos’ potential to grow – the percentage of pregnancies is the same as in the case of “fresh” embryos transfer.
Different IVF protocols
Short protocol
Takes place in a single menstrual cycle. There are two versions: antagonist protocol or hypothalamus analog protocol. Both are provided by injection, also in both cases, the patient’s ovulation is stimulated by gonadotropins.
Long protocol
Long protocol extends the procedure to two menstrual cycles. The first cycle is preparatory when the patient uses contraceptives, followed by downregulation with an analog (injections). It stimulates natural pituitary hormones, which stimulate ovulation. In the second menstrual cycle, the main stimulation starts: the patient takes gonadotropins by injection, and the analog treatment is prolonged.
EmbryoScope in IVF
System Time LapseTime Lapse Embryo Imaging – pioneering embryo monitoring systems. An EmbryoScope is an incubator that maintains the conditions for an embryo to thrive. The technology of the EmbryoScope allows specialists to monitor embryo cell divisions and development while the embryos stay in the incubator. Embryos stay in a stable environment, mimicking the inside of the body.
How does the EmbryoScope work?
The EmbryoScope uses a built-in camera and microscope, takes several pictures of the embryos every 5 minutes. This advanced technique allows embryologists to observe embryos in a stable environment and select those with the highest chance of implantation.
EmbryoScope allows:
- keeping embryos in a stable culture environment,
- constant monitoring of embryos development and more objective evaluation of their potential,
- to minimize the impact of external factors on embryos development,
- to lower the percentage of miscarriage,
- fully informed embryos selection,
- higher IVF success rates,
- constant observation of embryos, which leads to a better knowledge of cells division dynamics,
- presenting patients the whole process of embryo development from the moment of fertilization.





